HOW BONES MODEL AND REMODEL THEMSELVES
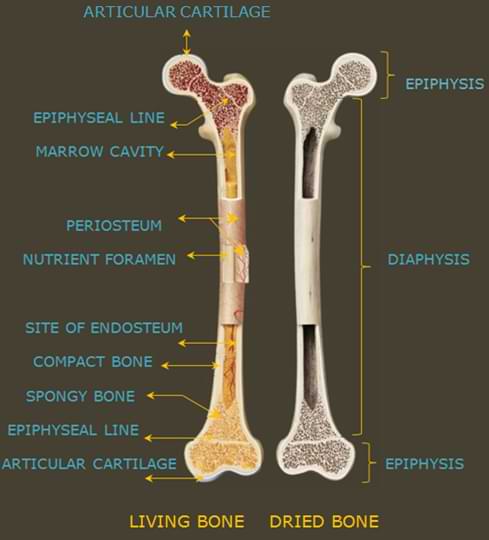
Anatomy of the human bone
Bone structure
Bone is composed of osteoid matrix (unmineralized, organic portion of the bone matrix that forms prior to the formation of compact bone), hydroxyapatite crystal (natural form of calcium apatite) and water.
Bones also contain proteins, lipids (fats) and specialized bone cells. [1]
The type 1 collagen bone matrix gives bone elasticity, flexibility and tensile strength.
The role of proteins in bone include strengthening the collagen structure and regulating its mineralization.
https://tinyurl.com/34eykktj
BONE TRANSFORMATION
Throughout life, the dynamic skeleton is constructed and renewed by two processes:
Bone modelling and Remodeling.
Both processes involve bone resorption ( break down and removal of old bone ) and bone formation.
During early childhood, both bone modelling and remodeling take place.
During childhood, the predominant process is the shaping and formation of new bone ( bone modeling ) while in adulthood, the replacement or renewal of old bone( bone remodeling ) is the predominant process except when a fracture occurs in which case, there is a rapid increase in bone formation. [2]
Bone modeling
Bone modelling is the process by which bones change shape or size in response to physiologic influences or mechanical forces that are encountered by the skeleton like exercises.
The bone lengthens and modifies by modeling, a process in which either bone breakdown or bone formation occurs on a given bone surface.
https://tinyurl.com/3xjt8p5x
During the process of modelling, bone resorption ( break down ) and formation occur independently at different skeletal sites to bring about major changes in bone architecture.
In the bone modeling process, bone is removed from one site and new bone is formed at another.
For instance, bone is removed from the metaphysis on the periosteal surface ( a membrane that covers the outer surface of all bones ) , while new bone is formed on the inner endosteal surface ( The inside surface of bones which border the bone marrow cavity ) thus converting the shape of the epiphysis into the diaphysis and increasing the length of bone.
Bone modelling also leads to the growth in width of the diaphysis of long bones in which case, resorption occurs on the endosteal surface, while bone formation occurs at the periosteal surface thus increasing the overall diameter of the bone.
https://tinyurl.com/2p93u8zp
The majority of bone modelling is completed by skeletal maturity but modelling can still continue among adults especially in an adaptive response to mechanical loading and exercise or in the case of the renal bone disease.
https://tinyurl.com/3y2fcsk5
Bone remodeling
Bone remodeling is a process by which the skeleton is continuously renewed to maintain the structural integrity or strength of bone.
Small zones of bone are broken down by osteoclasts and replaced by osteoblasts to ensure that structural integrity is maintained thereby replacing approximately 5 – 10% of the skeleton each year with the entire adult human skeleton replaced within 10 years. [3]
During this process, old bone is broken down and released into the blood stream in form of calcium and phosphorus to maintain a steady state of mineral concentration in the blood.
https://tinyurl.com/327wv4dk
Bone remodeling is a continuous process during which skeletal damage is repaired, accumulation of brittle hyper-mineralized bone is kept in check and mineral homeostasis is maintained by releasing stores of calcium and phosphorus into the bloodstream.
The overall bone volume and structure remain unchanged during this process.
Bone cells
There are four main types of cells that are active within bones.
1. Osteoblasts
These are the cells responsible for the manufacture and mineralization of new bone.
The process of bone formation begins with the osteoblasts manufacturing a protein matrix or mixture ( Osteoid ) which is made up of mainly collagen and other organic proteins.
The osteoblasts then deposit minerals like calcium into the protein matrix which are then solidified to manufacture bone.
After depositing the minerals, the osteoblasts are then buried within the bone matrix to become osteocytes.
Thus, before the organic matrix of bone or the young bone is mineralized, it is known as osteoid.
Hence, when osteoblasts produce osteoid at a higher rate, they can be stimulated to increase bone mass.
Manufacture of osteoid by osteoblasts is triggered by growth hormone release.
https://tinyurl.com/bddn84wt
2. Osteocytes
Osteocytes are simply osteoblasts that are no longer active. They form when osteoblasts become buried in the mineral matrix of bone.
They coordinate the actions of osteoblasts and osteoclasts via several mechanisms.
For instance, they squeeze out and release proteins that signal to osteoblasts, osteoclasts, and other bone-residing cells to respond to environmental changes.
Hence, they act as sensors when stress is applied to bones or in case of bone fractures, signaling osteoclasts to dissolve the bone.
https://tinyurl.com/2555xtkj
3. Chondrocytes
Cells that form cartilage including the growth plate cartilage and they also play a role when it comes to fracture repair.
https://tinyurl.com/54s43hhe
4. Osteoclasts.
The cells responsible for dissolving or breaking down old bones.
They achieve this by secreting an acid that destroys the bone matrix.
This role played by osteoclasts is very vital for bone remodeling which involves continuously removing and replacing bone tissue for structured growth and in response to mechanical stress applied to bones.
https://tinyurl.com/y4rfsfk5
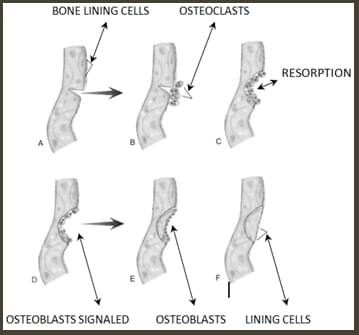
THE BONE REMODELING PROCESS / CYCLE
The remodeling cycle consists of five consecutive phases:
1. Activation
During this phase, an initiating remodeling signal is detected.
Day to day activities may increase mechanical strain on the skeleton, and it is hypothesized that when osteocytes sense the changes from the physical forces they express them into biological signals that initiate bone remodeling.
https://tinyurl.com/yzxdd4fs
The pre- osteoblasts which later fuse to form osteoblasts are then attracted from circulation to the remodeling site and activated.
It is conceived that the biological signals that trigger the formation of osteoclasts may stimulate the bone lining cells to prepare for bone resorption.
The bone lining cells then absorb a thin layer of non-mineralized bone to expose the mineralized matrix beneath.
Once the bone surface is exposed, a cover is raised over the bone site to be broken down.
https://tinyurl.com/3dhe9xaz
2.Resorption
During this stage, the osteoclasts attach to the bone surface, and a seal off a resorbing compartment.
hey then acidify the sealed compartment to dissolve bone mineral by secreting or pumping protons (H+ ions).
Once bone is dissolved, the organic matrix of bone (one that includes the collagen and ground substance)
is exposed to proteolytic enzymes ( enzymes that break down protein) that break it down.
During the resorption stage, both the bone matrix and bone mineral are digested.
https://tinyurl.com/yc5rbwe5
3. Reversal
The reversal stage begins after old bone has been eroded to the maximum depth.
During this stage, the osteoclasts die as the osteoblasts are recruited and begin to evolve.
https://tinyurl.com/szt2d8ty
Thus, this stage marks the transition from osteoclast to osteoblast activity.
https://tinyurl.com/4yvmekah
After the osteoclasts are evacuated from the resorption pit, preparation of the bone surface occurs when the bone-lining cells enter the lacuna and remove the mineralized collagen matrix from its bottom.
Cleaning the lacuna is a prerequisite for the subsequent deposition of a first layer of proteins in the resorption pits and form a cement line that helps in attaching of the osteoblasts.
4. Formation (Takes approx. 4 months)
This is the longest process and it’s slower than the bone resorption process because during this phase, both The bone formation and mineralization take place.
It takes approximately four months.
https://tinyurl.com/y2nucbuy
During this stage, osteoblasts first manufacture and release a type 1 collagen-rich osteoid matrix.
For bone to assume its final form, hydroxyapatite crystals ( naturally occurring mineral form of calcium ) are deposited into this newly deposited osteoid .
Non-collagenous proteins play a part when it comes to the process of matrix maturation, mineralization regulation of the functional activity of bone cells.
The composition of bone is approximately 10% cells, 60% hydroxyapatite crystals and 30% organic matrix.
Bone formation and the entire remodeling cycle concludes when an equal amount of bone that was broken down has been replaced.
https://tinyurl.com/yc5rbwe5
5. Termination
Upon completion of bone mineralization, the osteoblasts either transform into bone-lining cells, die or get buried within the bone matrix before transforming into osteocytes.
Please Share If you Like This Page Thanks…!